Connect With Us
Featured Articles

How Ankle Sprains May Affect Foot Stability and Strength

An ankle sprain, a common injury, occurs when the ligaments surrounding the ankle stretch or tear due to sudden twisting or rolling movements. While seemingly minor, neglecting proper treatment can lead to complications, notably ankle instability and diminished strength. An unstable ankle, characterized by a recurring feeling of giving way, poses risks of further injury and compromises mobility. This instability arises from weakened ligaments, which struggle to effectively support the ankle's weight-bearing function. Additionally, reduced ankle strength follows, as the muscles surrounding the ankle weaken from disuse during the recovery phase. Over time, this weakness can affect balance and movement, increasing the likelihood of future injuries. Consequently, comprehensive treatment that addresses both ligament healing and muscle strengthening is vital to restore stability and strength, ensuring optimal ankle function and minimizing the risk of recurrent sprains. If you have sprained your ankle, it is strongly suggested that you seek prompt attention from a podiatrist who can help you begin the healing process.
Ankle sprains are common but need immediate attention. If you need your feet checked, contact Dr. Thong V. Truong from California. Our doctor can provide the care you need to keep you pain-free and on your feet.
How Does an Ankle Sprain Occur?
Ankle sprains take place when the ligaments in your ankle are torn or stretched beyond their limits. There are multiple ways that the ankle can become injured, including twisting or rolling over onto your ankle, putting undue stress on it, or causing trauma to the ankle itself.
What Are the Symptoms?
- Mild to moderate bruising
- Limited mobility
- Swelling
- Discoloration of the skin (depending on severity)
Preventing a Sprain
- Wearing appropriate shoes for the occasion
- Stretching before exercises and sports
- Knowing your limits
Treatment of a Sprain
Treatment of a sprain depends on the severity. Many times, people are told to rest and remain off their feet completely, while others are given an air cast. If the sprain is very severe, surgery may be required.
If you have suffered an ankle sprain previously, you may want to consider additional support such as a brace and regular exercises to strengthen the ankle.
If you have any questions please feel free to contact our office located in Chico, CA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Ankle Sprains
Although ankle sprains may not be as serious as a broken ankle, they should be given immediate attention and care. An ankle sprain can lead to a significant amount of pain, as well as limited mobility. They are often characterized by the swelling and discoloration of the skin. This occurs when the ligaments are stretched beyond their limits.
The simple act of walking can sometimes cause a sprain, which makes ankle sprains a very common injury that can happen to anyone. They occur when the ankle twists in an awkward way or rolls over itself, causing a pop or snap in the tendons around the ankle. Some people are more at risk than others. These include athletes who continually push their bodies to the limits and also people who have previously suffered accidents to the feet, ankles, or lower legs.
Most of the time, an ankle sprain is not severe enough for hospital attention. There are many at-home treatment options available, including propping the leg up above your head to reduce blood flow and inflammation, applying ice packs to the affected area as needed, taking over-the-counter pain relievers and anti-inflammatory medication, using an ACE bandage to wrap and support the injured ankle, and most importantly, remaining off your feet until the ankle has fully healed.
Despite this, an ankle sprain can turn into a severe injury that might require hospitalization. If the ankle ligaments or muscles are damaged from a tear or rip, that is one sign that the sprain is severe enough for hospital attention and possibly for surgery. Even after the surgery, the recovery process can be long. You may need to have rehabilitation sessions administered by your podiatrist to get your ankle back to full health.
The severity of your sprain might become apparent if you are unable to stand or walk, consistent pain occurs over a prolonged period of time, swelling is much more severe than initially present, or if you start to experience tingling or numbness. These signs may indicate that your ankle sprain might actually be a broken ankle, an injury that requires immediate medical attention.
Although they are not completely avoidable, ankle sprains can be curbed with some preventative treatment measures. These include wearing appropriate-fitting shoes that not only provide a comfortable fit, but also ankle support. It is also recommended to stretch before doing any kind of physical activity, as this will help lower your body’s chance for an injury.
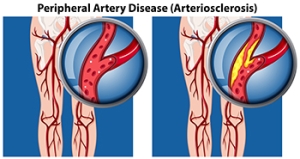
Managing Peripheral Artery Disease
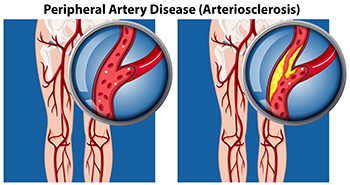
Peripheral artery disease, or PAD, particularly affects people with type 2 diabetes. Peripheral artery disease is often mistaken for normal aging or arthritis, but in fact it is the result of a build-up of fatty deposits in the arteries that restricts blood supply to the lower limbs and feet. Leg pain during exercise that persists with rest could signal PAD, necessitating evaluation by a podiatrist. Risk factors such as diabetes, smoking, and high cholesterol significantly contribute to PAD. Regular check-ups with a podiatrist, especially for diabetic individuals, are essential for assessing and managing foot health. One side effect of peripheral artery disease is the inability of wounds to heal properly, putting the patient at risk for foot ulcers. Early detection and intervention is essential, as such open wounds can deteriorate into gangrene and increase risk of limb loss if left untreated. For that reason, symptoms like persistent leg pain or slow-healing wounds require prompt medical attention from a podiatrist. If you are experiencing symptoms of peripheral artery disease, it is suggested that you add a podiatrist to your team of healthcare professionals.
Peripheral artery disease can pose a serious risk to your health. It can increase the risk of stroke and heart attack. If you have symptoms of peripheral artery disease, consult with Dr. Thong V. Truong from California. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Peripheral artery disease (PAD) is when arteries are constricted due to plaque (fatty deposits) build-up. This results in less blood flow to the legs and other extremities. The main cause of PAD is atherosclerosis, in which plaque builds up in the arteries.
Symptoms
Symptoms of PAD include:
- Claudication (leg pain from walking)
- Numbness in legs
- Decrease in growth of leg hair and toenails
- Paleness of the skin
- Erectile dysfunction
- Sores and wounds on legs and feet that won’t heal
- Coldness in one leg
It is important to note that a majority of individuals never show any symptoms of PAD.
Diagnosis
While PAD occurs in the legs and arteries, Podiatrists can diagnose PAD. Podiatrists utilize a test called an ankle-brachial index (ABI). An ABI test compares blood pressure in your arm to you ankle to see if any abnormality occurs. Ultrasound and imaging devices may also be used.
Treatment
Fortunately, lifestyle changes such as maintaining a healthy diet, exercising, managing cholesterol and blood sugar levels, and quitting smoking, can all treat PAD. Medications that prevent clots from occurring can be prescribed. Finally, in some cases, surgery may be recommended.
If you have any questions, please feel free to contact our office located in Chico, CA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Peripheral Artery Disease
Peripheral artery disease (PAD), or peripheral arterial disease, is a circulatory problem in which there is a reduction of blood flow to the limbs due to narrowed arteries. When peripheral artery disease develops, the extremities do not receive enough blood flow; this may cause symptoms to develop such as claudication, or leg pain when walking. The legs are the most common site of peripheral artery disease.
Claudication, or leg pain when walking, is one of several symptoms that can develop due to peripheral artery disease. Other symptoms caused by the disease include painful cramping in the hips, thighs, or calves after certain activities; leg numbness or weakness; coldness in the lower leg or foot; sores on the lower extremities that do not heal; hair loss on the lower extremities; and a missing or weak pulse in the lower extremities. In more severe cases, pain may even occur when the body is at rest or when lying down.
Peripheral artery disease is typically caused by atherosclerosis, a condition in which fatty deposits build up in the arterial walls and reduce blood flow. Smoking, diabetes, obesity, high blood pressure, and high cholesterol are some of the risk factors for peripheral artery disease.
If you are experiencing pain, numbness, or other symptoms in the lower extremities, see your healthcare professional immediately. Diagnosed peripheral artery disease can be treated with various medications, angioplasty and surgery, exercise programs, or alternative medicine. It is important to consult a healthcare professional to determine the best treatment for you.
Arthritis Can Cause Pain in the Feet and Ankles
Causes and Common Triggers of Heel Pain

Heel pain can stem from various factors, affecting individuals of all ages and activity levels. Primarily localized to the underside or back of the heel, this discomfort can significantly impact mobility and quality of life. The causes of heel pain are multifaceted, with common culprits including plantar fasciitis, Achilles tendonitis, heel spurs, and stress fractures. Plantar fasciitis, caused by inflammation of the thick band of tissue that connects the heel to the toes, often arises from overuse, improper footwear, or biomechanical issues. Achilles tendonitis, involving inflammation of the Achilles tendon, commonly results from overuse or sudden increases in activity level. Heel spurs, bony growths on the underside of the heel bone, can develop due to repetitive stress or poor foot mechanics. Stress fractures, small cracks in the heel bone, may occur from overtraining or sudden changes in activity. If you have heel pain, it is strongly suggested that you consult a podiatrist who can determine the cause and offer you appropriate relief and treatment solutions.
Many people suffer from bouts of heel pain. For more information, contact Dr. Thong V. Truong of California. Our doctor can provide the care you need to keep you pain-free and on your feet.
Causes of Heel Pain
Heel pain is often associated with plantar fasciitis. The plantar fascia is a band of tissues that extends along the bottom of the foot. A rip or tear in this ligament can cause inflammation of the tissue.
Achilles tendonitis is another cause of heel pain. Inflammation of the Achilles tendon will cause pain from fractures and muscle tearing. Lack of flexibility is also another symptom.
Heel spurs are another cause of pain. When the tissues of the plantar fascia undergo a great deal of stress, it can lead to ligament separation from the heel bone, causing heel spurs.
Why Might Heel Pain Occur?
- Wearing ill-fitting shoes
- Wearing non-supportive shoes
- Weight change
- Excessive running
Treatments
Heel pain should be treated as soon as possible for immediate results. Keeping your feet in a stress-free environment will help. If you suffer from Achilles tendonitis or plantar fasciitis, applying ice will reduce the swelling. Stretching before an exercise like running will help the muscles. Using all these tips will help make heel pain a condition of the past.
If you have any questions please contact our office located in Chico, CA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Heel Pain
Heel pain can be difficult to deal with, especially if you do not know what the underlying cause is. If you ignore your heel pain, the pain can magnify and potentially develop into a chronic condition. Depending on the location of your heel pain, you have developed a specific condition.
One condition is plantar fasciitis. Plantar fasciitis is caused by the inflammation of the plantar fascia, or the band of tissue that connects the heel bone to the base of the toes. The pain from this condition is initially mild but can intensify as more steps are taken when you wake up in the morning. To treat this condition, medication will likely be necessary. Plantar fasciitis is often associated with heel spurs; both require rest and special stretching exercises.
There are various options your podiatrist may suggest for heel pain. Treatment options for heel pain typically include non-steroidal anti-inflammatory drugs (NSAIDS), which may reduce swelling and pain. Other options are physical therapy, athletic taping, and orthotics. In severe cases of heel pain, surgery may be required.
Preventing heel pain is possible. If you are looking to prevent heel pain from developing in the future, be sure to wear shoes that fit you properly and do not have worn down heels or soles. Be sure to warm up properly before participating in strenuous activities or sports that place a lot of a stress on the heels. If you are experiencing any form of heel pain, speak with your podiatrist to determine the underlying cause and receive the treatment you need.
Recognizing Symptoms of Plantar Fibroma

Plantar fibroma, a benign tissue growth that develops on the bottom of the foot, can cause discomfort and affect mobility. Recognizing the symptoms of plantar fibroma is essential for early diagnosis and effective management. One common symptom is the presence of a firm, palpable nodule or lump in the arch or midfoot region. This nodule may vary in size and can be tender to the touch, causing pain or discomfort, especially when standing or walking. Some individuals may also experience a sensation of pressure or tightness in the affected area, particularly when wearing tight or constrictive footwear. As the plantar fibroma progresses, it may lead to changes in foot structure and function, such as difficulty bearing weight on the affected foot or altered gait patterns. If left untreated, plantar fibromas can worsen over time, potentially causing chronic pain and interfering with daily activities. If you have noticed a lump on the sole of your foot, it is suggested that you visit a podiatrist who can properly treat this condition.
A plantar fibroma may disrupt your daily activities. If you have any concerns, contact Dr. Thong V. Truong of California. Our doctor can provide the care you need to keep you pain-free and on your feet.
Plantar Fibroma
A plantar fibroma is a fibrous knot in the arch of the foot. It is embedded in the plantar fascia which is a band of tissue that extends from the heel to the toes along the bottom of the foot. There can be multiple plantar fibromas in the feet at the same time. There are no known causes for this condition. If you have a plantar fibroma, there will be a bump in the arch of your foot that cannot be missed. Any associated pain is most often due to a shoe rubbing against the nodule. Non-surgical options, such as steroid injections, physical therapy, and orthotics should be tried first. Surgery is a last resort and is the only thing that will remove a plantar fibroma entirely. Consult with a podiatrist for a proper diagnosis and to determine the treatment regimen that is right for you.
What Causes a Plantar Fibroma?
While there are no specific causes identified, a plantar fibroma can possibly come from genetic predisposition or the formation of scar tissue that forms from healing the tears in the plantar fascia.
What Are the Symptoms of a Plantar Fibroma?
There will be a noticeable lump in the arch of the foot that may or may not cause pain. If pain is felt, it is typically because a shoe is rubbing up against the lump or when walking or standing barefoot.
Treatment and Prevention
A plantar fibroma will not disappear without treatment, but it can get smaller and be a non-issue. If pain persists, a podiatrist examines the foot and when the arch of the foot is pressed, pain can be felt down to the toes. An MRI or biopsy might be performed to help diagnose or evaluate the plantar fibroma. The following non-surgical options are generally enough to reduce the size and pain of these nodules:
- Steroid injections
- Orthotics
- Physical therapy to help apply anti-inflammatory creams on the bump
Surgery is considered if the mass increases in size and the patient continues to feel pain after non-surgical methods are tried.
If you have any questions please feel free to contact our office located in Chico, CA . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.